Mental Health Association of Rockland County Inc. has agreed to pay $304,000 to resolve claims in a lawsuit against the organization regarding Medicaid record keeping, the office of state Attorney General Eric T. Schneiderman announced on Monday.
The nonprofit, which provides outpatient mental health services to children and adults in Rockland County, admitted that prior to a Medicaid audit in 2009, employees made handwritten changes to records so they would appear to support claims the organization submitted to the state’s Medicaid program, the attorney general’s office reported. In the days preceding the October 2009 audit, managers and employees at the organization made more than 40 handwritten changes to progress notes that were completed between 2003 and 2008, the AG’s office said.
Under the state False Claims Act, New York can recover penalties relating to the creation or use of false records in connection to Medicaid claims. About $250,000 of the $304,000 settlement is to resolve claims for penalties under the state and federal false claims acts. The remainder of the settlement resolves claims relating to MHA Rockland’s failure to have progress notes or treatment plans for certain Continuing Day Treatment program participants, in violation of Medicaid program regulations.
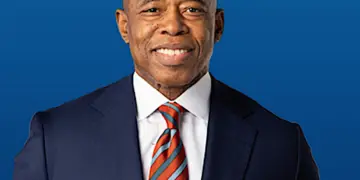
“Audits are an important tool in protecting Medicaid funds that should be used to provide health care to millions of New Yorkers,” Schneiderman said in a statement. “Any attempt to undermine those audits and our Medicaid program will be investigated aggressively by my office.”
The attorney general’s investigation was prompted by the filing of a whistleblower lawsuit by two former MHA Rockland employees, who will receive a portion of the settlement.
The state Office of the Medicaid Inspector General and the U.S. Attorney’s Office for the Southern District of New York assisted with the investigation.