From a research campus in Irvington on the former estate of a son of Alexander Hamilton, Columbia University Medical Center researchers aim to investigate a new treatment for pancreatic cancer.
Pancreatic cancer is still considered largely incurable and is expected to become a leading cause of cancer deaths in the U.S. The cancer is often discovered late, limiting treatment options. Columbia University Medical Center recently was awarded a $400,000 state grant to help fund its study of a new form of treatment that has shown positive trial results overseas.

“While there have been super advances in all the other major cancers we face, in prostate cancer, breast cancer and, to an extent, lung cancer too, there have been no advances really in the past 20, 30 years for pancreatic cancer,” said David J. Brenner, director of Columbia University Medical Center”™s Center for Radiological Research. “So, while all the other death rates are going down ”” lung, breast, prostate ”” pancreas is actually going up.”
The five-year survival rate for patients diagnosed with the cancer improved from just 2.5 percent in 1975 to 8.5 percent in 2012 in the U.S., according to the National Institutes of Health, near lowest among the most common cancers. About 43,000 Americans died of pancreatic cancer last year, according to estimates from the American Cancer Society.
“Soon enough pancreatic cancer is going be the No. 2 cancer killer, behind lung,” Brenner said. That has pushed researchers to find some kind of response, he said.
At Columbia University Medical Center, researchers have been tracking the results of a new type of treatment administered in Japan. There, carbon-ion radiation therapy has produced unusually strong results in treatment trials.
The much-heavier carbon ions damage both DNA and cancer cells in different ways than more common types of radiation therapy, such as X-ray and proton, Brenner said.
While the U.S. does not have a carbon-ion radiotherapy facility, there are such facilities in Japan and Germany. In a trial study in Japan, 50 percent of patients survived two years after a pancreatic cancer diagnosis when treated with carbon-ion radiation therapy. The typical two-year survival rate is 25 percent.
“That”™s unusual in the cancer therapy world, where things move rather more incrementally than that ”” little gains, little gains, little gains,” Brenner said. “So that certainly caught people”™s attention and caught our attention. What we wanted to do, initially, is figure out, well what”™s going on?”
The results were especially striking because, after two years, people with pancreatic cancer typically die from the cancer metastasizing to other parts of the body.
“In general, you wouldn”™t expect radiation to be very helpful in that context,” Brenner said. “Because with radiation you try to target the tumor as accurately as you possibly can. You”™re not irradiating the rest of the body. So how is it that there is this really good survival after two years when people would be expected to die of distant metastases?”
One theory that the Columbia researchers plan to test is that the radiation is triggering some type of body-wide immune response, similar to immunotherapy treatments for other cancers that stimulate a patient”™s immune system to attack cancer cells.
“In other contexts, people are thinking a lot about immunotherapy for cancer, so our strong suspicion is that what is going on here,” Brenner said. “But that”™s by no means proven and there isn”™t really any research going on as to why this is so good.”
That”™s where Columbia”™s facility in Irvington enters the picture. Down a leafy, single-lane private road off Route 9 in Irvington is Nevis Laboratories, a 68-acre research campus for Columbia University and Columbia University Medical Center. The property dates to James Hamilton, a son of Alexander Hamilton, who named the estate Nevis after the small Caribbean island where his father was born.
The younger Hamilton built a Greek revival mansion in 1835, which still stands and houses visiting researchers.

The property stayed in the family until the early 20th century. In 1920, it was purchased by Thomas Coleman du Pont, an early president of the DuPont company and a Republican U.S. senator from Delaware. In 1934, du Pont”™s widow donated the estate to Columbia University, which converted it to its main physics research campus.
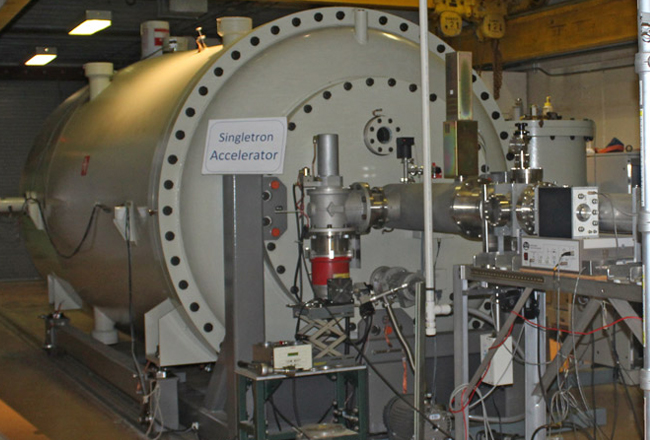
Part of that research campus is RARAF, the Radiological Research Accelerator Facility. It houses the only particle accelerator in the country dedicated to radiological research. RARAF is part of Columbia”™s Center for Radiological Research, founded in 1916 to study the impact of radiation exposure on human health.
The accelerator research started at Brookhaven National Labs on Long Island but moved to the Columbia Irvington campus in 1984. The accelerator has been a research hub for Columbia”™s Center for Radiological Research as well as outside researchers from universities, national laboratories, cancer centers and private corporations.
The accelerator could allow scientists to search for a better understanding of the mechanism behind carbon-ion radiation therapy. But to do that, the accelerator at RARAF will need a boost. It is capable of creating a microbeam strong enough to irradiate individual cells in a lab setting, but not to penetrate bodily tissue, such as will be needed for the mice testing that Columbia plans to start with. RARAF researchers need a linear accelerator booster to create enough energy in the accelerator”™s beam to start preclinical trials.
“We can start looking at the mechanisms of how it is that carbon ions are producing what we believe to be long-range immunological responses in a way that protons or X-rays clearly don”™t,” Brenner said.
Researchers would track the response to heavy-ion radiation therapy, including how the tumor reacts and whether there is evidence of an immunological response to the treatment in areas not radiated.
Along with the impact of treatment, researchers would test how it should best be administered and whether different particles could be as effective. Oxygen ions, helium ions or lithium ions are all possibilities, for example.
The heavier the ion, the more expensive the treatment would be to administer, Brenner said. “So, if helium ions could do the trick as well as carbon ions, that would be orders of magnitude less expensive.”
The expense is important, as Brenner said the current equipment required for carbon-ion therapy is too expensive and large for even a hospital setting.
A parallel phase of Columbia”™s research into heavy-ion therapy would involve designing accelerators that are smaller and cheaper. Columbia estimates that if the treatment proves effective, it could develop these devices for treatment centers around the country to help treat 50,000 patients a year. That”™s the number of people who not only have pancreatic cancer, but other forms of metastatic cancers as well.
“What we see happening is that it”™s not just going to be a potential cure, we hope, for pancreatic cancer, but for the other cancers where the cancer has metastasized to other parts of the body,” Brenner said. “We want to be able to stimulate the immune response and attack those metastases distant from the original tumor.”
The linear accelerator needed for Columbia to start research costs $2 million. Columbia University has committed to $150,000 on top of the $400,000 grant from the state. The rest would be raised through supporter donations.




















