Throughout history, infertility has generally been considered a woman’s problem. (Remember Henry VIII, desperate for a male heir, and his six put-upon wives? Historians now believe Henry may have had the Kell antigen, a protein that triggers immune responses, making him a poor reproductive match for his partners and explaining his physical and mental deterioration.)
In 60% of couples, infertility stems from male trouble, not female problems, with 1% to 2% of all men having no sperm in their ejaculate (azoospermia). Another 1% to 2% will have so few sperm (cryptospermia) that they cannot be counted on even for an in vitro fertilization (IVF) cycle.
October marked the fifth anniversary of a ground-breaking medical procedure in the United States that is now responsible for 36 babies born and a total of 50 pregnancies in couples where men who had no sperm or virtually no sperm in the ejaculate – some of whom had previously undergone traditional, invasive therapies to locate and identify sperm that failed — were able to father a child.
Developed in Israel, Extended Sperm Search and Microfreeze (ESSM) has brought results to men struggling with infertility. Maze Men’s Health in Harrison is the only medical practice in the U.S. performing this technique, seeing male patients from all over the world to have their semen analyzed and sperm located and frozen.
The results say it all:
- Since October 2019, Maze Men’s Health has performed 750 sperm searches through ESSM.
- With ESSM, Maze’s overall sperm recovery rate has been 40% for men with azoospermia and more than 90% for men with cryptospermia.
- Total IVF cycles in progress using sperm found via ESSM at Maze – 23.
- Total live births as a result of ESSM at Maze – 36.
- Total patients who released sperm to IVF labs – 51.

How ESSM works
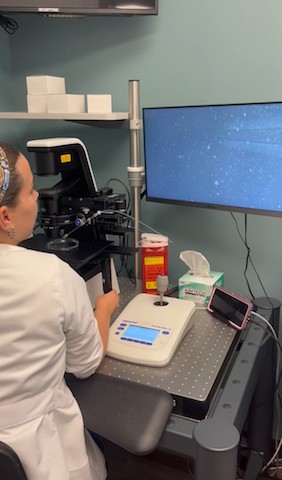
ESSM finds and freezes small numbers of sperm in men with azoospermia or cryptospermia. The entire semen sample is divided into microdroplets and carefully scanned under a high-powered microscope. Then Maze spends up to eight hours looking for sperm. Any sperm that are located are placed in a special device called SpermVD, which allows individual sperm to be transferred to a microdroplet for freezing and then cryopreserved for use in intracytoplasmic sperm injection (ICSI-IVF).
The ESSM process to divide the concentrated semen into droplets stemmed from a 2017 study by the Male Fertility Center in Tel Aviv, which found that examining the concentrated semen samples that comprise the entire sample, which is equivalent to 20 times the volume analyzed in a standard semen analysis, ultimately allows the physician to find rare sperm about 40% of the time. This new technique was then named Extended Sperm Search.
The second component of ESSM is the microfreezing, which overcomes two problems associated with traditional sperm freezing methods. First, the sperm survival rate with microfreezing is much higher than with standard freezing. Second, since traditional freezing is performed on much larger volumes of semen, once the larger sample is thawed, that an additional search must be performed to find the sperm within the sample. Since IVF is time-sensitive, the additional time required for the extra search presents additional challenges.
Because the sperm are successfully frozen in such a small quantity of fluid with ESSM, over 90% of them survive the freeze and thaw process. This process also makes the sperm easier to find when thawed on the day they are needed to inject into their partner’s egg (ICSI).
According to a 37-year-old patient, “I was told I was azoospermic after going to several well-known fertility centers in the tristate area. I then came to Maze for a standard semen analysis, which also showed zero sperm count. However, after having Maze’s ESSM lab test, 42 sperm were recovered and safely stored. In collaboration with the IVF lab, my wife and I are happy to say that seven healthy embryos were developed.”
The physicians at Maze suggest that ESSM should be performed prior to considering testicular sperm extraction, because ESSM is noninvasive and can be done as many times as needed. Contrarily, the traditional surgical extraction procedure called Testicular Sperm Extraction (micro-TESE) is invasive and may cause some damage to the testicles, reducing testosterone production, and thus can only be performed a limited number of times.
How much does ESSM cost?
Although ESSM pricing can’t be compared to standard sperm freezing, because the workflow is so different, it is significantly less than the cost of a surgical sperm extraction. For example, it costs $2,000 for the search and $100 per vial for freezing and is comparable to the laboratory fees for egg banking. Since ESSM is relatively new, it doesn’t fall into any of the existing codes used by insurance companies and is therefore not typically covered. However, each company is different, and Maze’s billing specialists work directly with each insurance company on behalf of its patients to discuss coverage options.
We are proud of the fact that we have profoundly changed the way we treat azoospermic and cryptospermic men. With these groundbreaking techniques, there will be more pregnancies with dramatically less intervention. The effect that ESSM will have on these couples trying to conceive will continue to be even more far-reaching and life-changing.

Michael A. Werner, MD, FACS, a board-certified urologist, is founder and medical director of Maze Health, which includes Maze Men’s Health, Maze Laboratories and Maze Women’s Health, with offices in Harrison and Manhattan. For more, click here. https://www.mazehealth.com/






















