Seeking a cure: Regeneron and NYMC in COVID-19 study
When a complex process that normally takes seven to nine months is accomplished in only eight days, you can be reasonably certain that something quite special has just happened.
That certain something is establishing the clinical trial of a drug that might help treat people critically ill with COVID-19. At present there are no vaccines for the novel coronavirus.
The U.S. Food and Drug Administration along with experts in medicine, pharmaceuticals, education, finance, data collection and more joined to slash through red tape and arrange the rapid launch of a clinical trial organized by a team at Touro College and University System and New York Medical College (NYMC) in Valhalla and Regeneron Pharmaceuticals along with the French multinational pharmaceutical company Sanofi.
Tarrytown-based Regeneron and Paris-based Sanofi had jointly developed under a global collaboration agreement the drug sarilumab, a monoclonal antibody known under the trademark Kevzara. Given by injection, the drug is approved for use to treat adult patients with moderately to severely active rheumatoid arthritis.
Kevzara binds to a protein associated with the human immune system called the Interleukin 6 receptor, or IL-6, which falls into the cytokine category. By inhibiting the ability of IL-6 to stimulate an immune system response, the drug inhibits inflammation.
The clinical trial is to test the drug as a possible COVID-19 treatment. In the trial, “severe” patients require supplemental oxygen without mechanical help or high-flow oxygenation. “Critical” patients need to be on high-flow oxygen or a mechanical ventilator.
Preliminary data released April 27 by Regeneron and Sanofi on Phase 2 of the trial classifies the COVID-19 results so far for the “severe” group of patients as “better than expected based on prior reports, regardless of treatment assignment.”
The companies said that in the Phase 2 portion, approximately 80% of the hospitalized patients were discharged, 10% died and 10% remained hospitalized.
The involvement of NYMC in the clinical trial began to unfold in March. Regeneron reached out to Dr. Alan Kadish, president of the Touro College and University System to see if the biomedical research team at Touro/NYMC would be interested in setting up a drug trial in the search for a way to treat COVID-19. The novel coronavirus was spreading around the world, had no known treatment, no vaccine and a fatality rate about 10 times that of influenza. NYMC not only has virology labs and experts, but for decades has been involved in the annual development of the influenza vaccine.
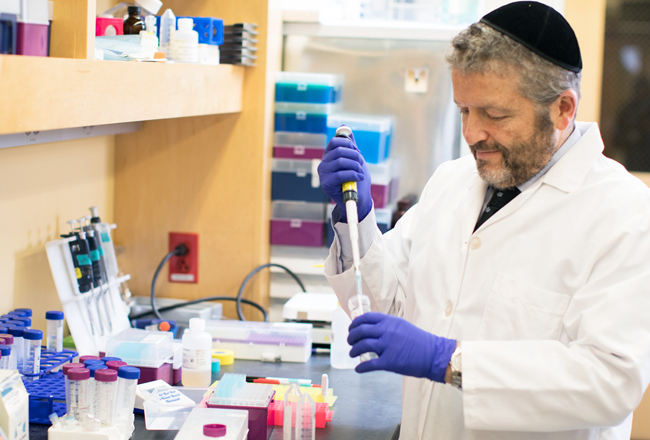
“It”™s an ongoing relationship that we had with Regeneron and Sanofi,” Dr. Salomon Amar told the Business Journal. He is the provost for biomedical research at Touro College and University System and professor of pharmacology, professor of microbiology and immunology, as well as vice dean for research at NYMC.
“We started a long-term collaboration at different levels on research and development, from basic science to clinical trials. It is a natural progression of this relationship with Regeneron that led them to ask us to participate in this program,” Amar said.
“We are talking about a viral particle that was unknown to us. We did not have any background information. Viral particles in general are contagious but this is highly contagious. The spread has taken us aback a little bit. If the person is a little bit immune compromised or a little bit obese or not able to mount a proper inflammatory reaction, in this case it is going to be devastating.”
Patients suffering from advanced cases of COVID-19 can experience breathing problems associated with inflammation affecting the lungs. In serious cases, what”™s known as a “cytokine storm” takes place. It”™s a dramatic response by the body”™s immune system that makes the lungs unable to function normally. The lungs become overrun by immune cells and fluid buildup, often leading to secondary bacterial pneumonia. Instead of being spongy and flexible, the lungs become febrile and oxygen can no longer be efficiently transferred across the lung tissue and into the blood. Patients with serious cases of COVID-19 need to be on supplemental oxygen. If lung function continues to deteriorate, patients need to be put on a ventilator or other breathing assistance device and survival can be in doubt. Approximately 80% of the patients requiring intubation do not survive.
If there is a way to reduce inflammation and relieve the cytokine storm, patients should be able to survive, so the thinking went. Regeneron and Sanofi theorized that since Kevzara relieved inflammation with arthritis, it might do the same with COVID-19. There had been a small uncontrolled test of the drug in China and it seemed to help.
“Emerging evidence with Kevzara and other repurposed drugs in the COVID-19 crisis highlight the challenges of making decisions about existing medicines for new viral threats using small, uncontrolled studies,” Regeneron co-founder George Yancopoulos said in a statement. “We await results of the ongoing Phase 3 trial to learn more about COVID-19, and better understand whether some patients may benefit from Kevzara treatment.”
Designing a clinical trial involves not only establishing scientific and research parameters but doing lots of paperwork, complying with regulations, arranging to recruit participants and working very closely with the site of the trial. For NYMC, the site was to be Westchester Medical Center (WMC), also in Valhalla.
“It”™s a multicenter study, not only at Westchester,” Amar said. “There are multiple sites in the United States as well as outside of the country. The NYMC involvement deals with what is happening at Westchester.”
Amar said that he could not provide the number of patients who are enrolled at the WMC because it is a blind study, meaning that patients and even the staff do not know who is getting the Kevzara and who is getting a placebo and what preliminary data is showing.
Regeneron and Sanofi in a public statement reported that the Phase 2 portion of the trial assessed 457 hospitalized patients who were categorized as having either “severe” illness or “critical illness or multi-system organ dysfunction.”
Amar explained that in this blind study, the patients are divided into three groups. One group does not receive Kevzara, but does receive a placebo, a nonactive substance, in addition to receiving the accepted standard of care. A second group receives 200 milligrams of Kevzara along with the accepted standard of care. The third group receives 400 milligrams of Kevzara, also with the accepted standard of care.
“In the case of COVID, we do not leave the patient without any treatment at all,” Amar said. “Everybody receives the standard of care. In the study, it”™s the standard of care plus the experimental drug or the standard of care with nothing. We compare the effect on two populations.”
Amar said it was hypothesized in the beginning that the drug would be more effective for patients with advanced cases because those patients are contending with more inflammation.
“Without any background information about how the disease progresses it is very difficult to design a study. So, we need to leave it open and we do some measurements midterm, called midterm or midlevel analysis, by looking at some parameters to see whether the parameters have changed or not changed. While the trial is being conducted it is called an open trial,” Amar said.
Regeneron and Sanofi announced that they have amended the trial for Phase 3 so that only “critical” patients will continue to be enrolled. Those patients will receive either the standard of care plus 400 milligram doses of Kevzara or the standard of care and a placebo.
“These initial results from the randomized clinical trial setting provide physicians much needed insights and information regarding the potential of Kevzara for patients with COVID-19 treatment,” said John Reed, Sanofi”™s global head of research and development.
Amar said that at some point, statisticians will have enough data to analyze and reach a conclusion about the effectiveness of the drug. If it is actually demonstrated to be safe and effective for treating COVID-19, FDA approval can be sought to have the drug labeled and marketed for use as a COVID-19 treatment.
“The trial was designed pretty elegantly given the circumstances and the parameters that we were operating with,” Amar said. “I am proud of the fact that everyone came to work Sundays, holidays. Everyone worked diligently and pulled together for the betterment of the situation.”